Myxoedema coma secondary to severe hypothyroidis
DOI:
https://doi.org/10.51496/jogm.v4.S1.161Keywords:
Myxoedema, Hypothyroidism, Covid, Clinical featuresAbstract
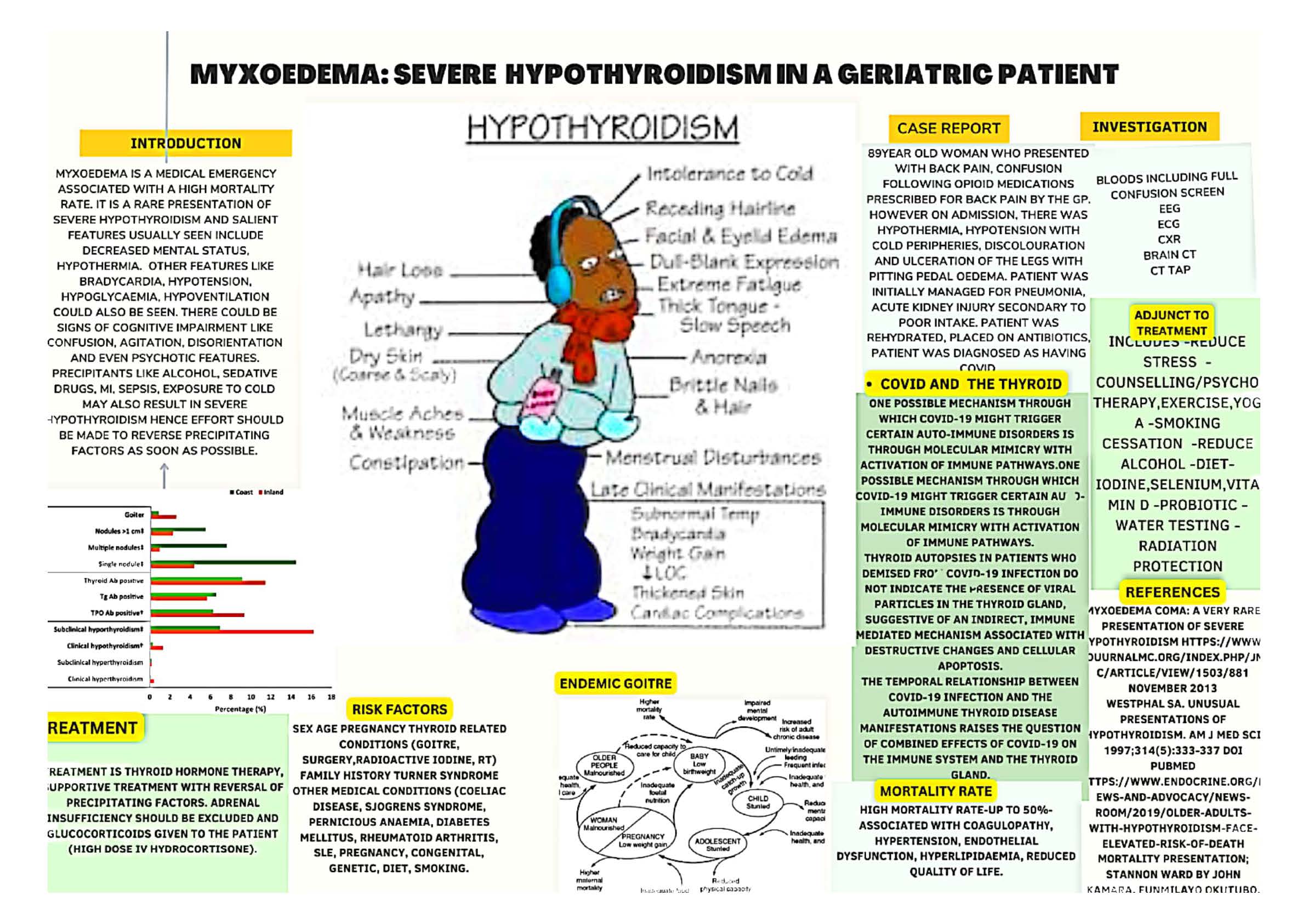
Introduction: Myxoedema is a medical emergency associated with a high
mortality rate. It is a rare presentation of severe hypothyroidism and
salient features usually seen include Decreased Mental Status,
Hypothermia. Other features like Bradycardia, hypotension, hypoglycaemia,
hypoventilation, signs of cognitive impairment like confusion, agitation,
disorientation, and even psychotic features could be seen.
Precipitants like alcohol, sedative drugs, MI, sepsis, exposure to cold may
also result in severe hypothyroidism; hence effort should be made to
reverse precipitating factors rapidly.
The incidence of Myxoedema Coma is very low in developed countries
as there is improved diagnosis and treatment; early, aggressive treatment
is necessary due to the high mortality rate (30–60%). Groups of patients
at risk include elderly patients, those with a compromise cardiovascular
system, reduced consciousness, sepsis etc. usually have a poorer outcome.
Mainstay of treatment is thyroid hormone therapy, supportive-reversal
of precipitating factors. Adrenal insufficiency should be excluded; glucocorticoids
are given to the patient.
Case report-discussion & results: I present an 89-year-old woman who presented
with Back Pain, Confusion following opioid medications prescribed
by the GP. However on admission, there was hypothermia,
hypotension with cold peripheries, pedal discolouration and ulceration,
pitting oedema. The patient was initially managed for pneumonia, acute
kidney injury secondary to poor intake. Patient was rehydrated and
placed on antibiotics. ECG, Transthoracic Echocardiography, Chest
X-Ray, Blood tests, Brain CT showed nil tumour or acute changes. CT
TAP showed nil malignancy or bony changes.
Few days following admission to the ward, patient tested positive
for COVID and was isolated. Following COVID Stepdown, the patient
developed altered sensorium, hypotension, and seizures. Lactate was
high, EEG showed nil evidence of encephalitis. A confusion screen which
included Thyroid Function Test (TFT) was requested. The lab called in
a few hours later due to a very high level of TSH (63) and low T4 (5.1)
and Levothyroxine was commenced. Referral was made to the endocrinologist.
Gentle rewarming using blankets with the room heater at room
temperature was done and the patient was also placed on antibiotics.
Relatives were updated as events evolved, and diagnosis changed with
time. Repeat TFT showed that the TSH level increased and there was clinical
worsening of the patient’s mental state. A diagnosis of Myxoedema
coma was made.
Conclusion: A low threshold for requesting investigations like TFT, especially
in at-risk patients and a high index of suspicion is required clinically.
Could Covid have contributed to the precipitating factors? A
referral was made to the Palliative Care Team. There was good multidisciplinary
team input with relatives updated from time to time with mention
of limited prognosis.
Metrics
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Funmilayo Okutubo

This work is licensed under a Creative Commons Attribution 4.0 International License.






 Journal of Global Medicine | Editor-in-Chief: Olufunso Adedeji. MBBS, MD, FRCSEd.
Journal of Global Medicine | Editor-in-Chief: Olufunso Adedeji. MBBS, MD, FRCSEd.